Beyond Tissue Damage: Understanding Central Sensitization & Chronic Pain
By: Nataliya Zlotnikov, MSc, HBSc ∙ Estimated reading time: 5 minutes
By: Nataliya Zlotnikov, MSc, HBSc ∙ Estimated reading time: 5 minutes
Introduction: Pain Threshold
Let us start this blog with a somewhat contentious question, the answer to which may be surprising to some:
Who has a higher pain threshold, men or women?
Neither! From a biological standpoint, both sexes have the same pain threshold; however, most perceive their own sex to possess the superior pain threshold.
![]()
What is perhaps most amusing is that men do have a higher pain threshold,
if their researcher is an attractive female.
However, in women, the researcher does not seem to make a difference.
Some studies do show that women have a lower pain threshold compared to men because women are more likely to experience anxiety issues, and anxiety reduces pain threshold.
But, under conditions of the same psychosocial status, men and women have the same threshold.
As a clinician, before determining if and what physiotherapy intervention is most appropriate for a patient, the possible source of the patient’s pain must be hypothesized.
This blog is based on Bahram Jam's course APTEI: Pain Truth Certification Training.
Pain Truth Certification Training Course Learning Objectives:
-
If and what physical therapy intervention is most appropriate for a patient with persistent pain.
-
The latest evidence, treatment management strategies, and the use of mindful movements in patients with central sensitization or centrally sensitized pain (CSP).
- The most up-to-date interventions for their patients with central sensitization.
Learn What Else This Course Offers:
Explore the full course on Embodia
And now, a sneak preview of some of the course content:
Three Classifications of Pain:
There are three classifications of pain:
Nociceptive pain (NP), peripheral neurogenic pain (PNP) and central sensitization pain (CSP).
Additionally, there is also visceral pain (e.g. pain from kidneys, colon, etc.); however, the latter falls beyond the scope of our practice.
Let us discuss each of the three pain types in a little more detail:
- Nociceptive pain (NP). This is the pain that newly graduated physiotherapists often believe all patients have. Any structure that is innervated with nociceptors, such as your muscles, bones, tissues and ligaments, can be a source of NP. For example, spraining your ankle or fracturing your wrist would both result in NP.
- Peripheral neurogenic pain (PNP). PNP occurs when you have an irritation, sensitization, or compression of an S1 or C5 nerve root and get numbness or tingling. PNP is neural pain, and, as physiotherapists, we are good at identifying this kind of pain.
- Central sensitization pain (CSP). CSP does not fall into either of the above groupings, and will be discussed in slightly greater detail in this blog and more deeply in Bahram Jam’s webinar: APTEI: An Introduction to the Pain Truth Certification Program, upon which this blog is based.
Now that we have discussed the three classifications of pain, let us look at three sets of pain diagrams:

At first look, you would say that the person on the left has nociceptive pain, the middle person has peripheral neurogenic pain, and the last person has fibromyalgia or centrally sensitized pain.
But if only life were that easy!
Could the person on the left with localized lumbar pain also have centrally sensitized pain?
YES!
Can the middle person also have CSP?
YES!
And can the rightmost person, the person with CSP, can that person have nociceptive pain as well?
Also YES!
As if that didn’t complicate things already, we also know that all three pain types are influenced by emotions.
Stress, anger, depression, anxiety, avoidance beliefs, catastrophizing, job dissatisfaction and reduced hopefulness are all known to impact our pain.
More specifically, all three pain classifications are further aggravated by anxiety.
As physiotherapists, we cannot be judgmental about regional pain to decide what classification of pain a person has; we need more information!
![]()
As physiotherapists, we cannot be judgmental about regional pain to decide
what classification of pain a person has;
we need more information!
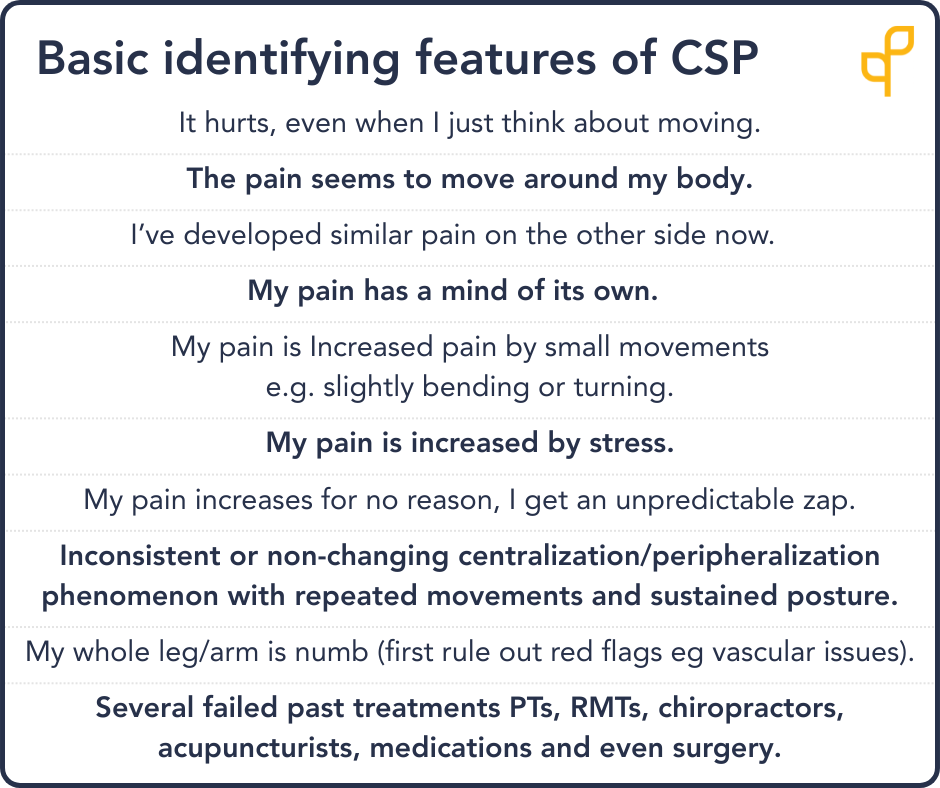
Can We More Confidently Identify CSP?
If we cannot trust pain diagrams and medical imaging alone, what can we trust to identify CSP?
We can use the GIQ 12, an intake questionnaire created by Bahram Jam, founder of the Advanced Physical Therapy Education Institute (APTEI).
Bahram confesses that GIQ 12 is not reliable, it is not validated, but it doesn’t need to be.
It is not an outcome measure; it is simply an intake questionnaire that aids in identifying CSP.
Bahram uses this questionnaire with all his patients, whether they have suffered an ankle sprain or have been dealing with fibromyalgia for five years.
Using this questionnaire, he can confidently determine whether a patient is centrally sensitized or not.
Click here for Bahram's course
Identifying the 3 Classifications of Pain:
- Nociceptive pain (NP): NP is associated with pain from any anatomical structure that has a nerve supply. NP is localized to the area of injury, has predictable aggravating and relieving factors, and is influenced by movement or posture. Persons suffering from NP pain respond well to physiotherapy. Their condition improves with manual therapy, soft tissue release techniques, and rest.
- Peripheral Neurogenic Pain (PNP): PNP is associated with pain related to neural tissue inflammation, compression and or pathology. The pain is deep, knife life, sharp and follows a linear pattern. These patients would have a positive slump and straight leg test.
- Central Sensitization Pain (CSP): CSP is associated with chronic pain states and is due to the sensitization of the central neurons leading to decreased threshold to all normal afferent input i.e. fibromyalgia, phantom limb pain, chronic spinal pain, chronic WAD.
Does one type of pain exclude the other?
The pain classifications can overlap; however, central sensitization will trump the remaining two classifications.
For example, a normal person will feel some knee pain as a tweak in their knee, whereas people who are centrally sensitized will feel greatly magnified symptoms.
In CSP, the nociceptive pain is heightened way above the usual threshold, and this disables the patient; this is further aggravated by fear and anxiety.
Why Identify CSP?
It is essential for PTs to identify CSP, as focusing on treating specific anatomical structures is likely futile.
In fact, treatments such as pain-relieving modalities, pain medications, specific manual therapy, and specific localized exercises may all exacerbate the cerebral cortex’s focus on pain and even further contribute to chronicity.
![]()
Manual therapy-specific exercises will make central sensitization worse!
There IS a place for manual therapy and exercises, just not with chronic pain.
Summary
As clinicians, we place the safety and well-being of our patients above all else.
Gaining a better understanding of central sensitization pain (CSP), we become aware of why certain treatments may not have worked for some of our patients in the past.
To effectively treat patients with CSP, we must work in a different way.
Based on the best available evidence to date, the strategies for treating CSP are dramatically different from those we use to treat nociceptive pain (NP) and peripheral neurogenic pain (PNP).
---
Date written: 25 May 2020
Last update: 18 December 2025
PT, D.SC.PT, M.PHTY, B.SC.PT, FCAMT
Bahram is a physiotherapist and founder of the Advanced Physical Therapy Education Institute (APTEI). He's taught 1000+ continuing education courses to healthcare professionals across Canada & internationally.
He has instructed over one thousand post-graduate orthopaedic and pain science courses and has been a guest presenter at several physiotherapy and medical conferences across Canada and internationally.
His primary clinical approach is to identify relevant functional impairments and determine the best self-management strategy to maximize patient independence.
